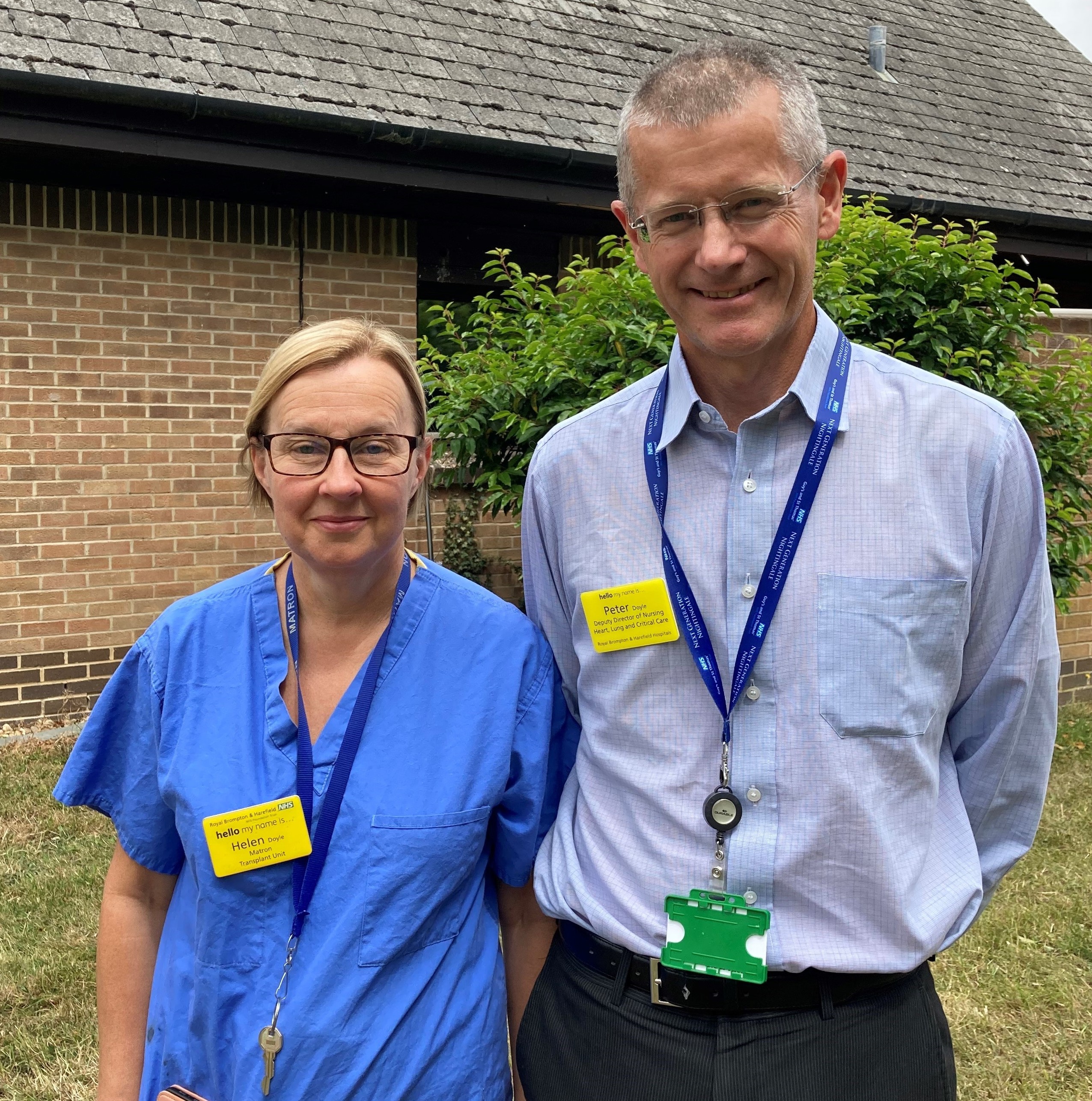
Helen Doyle, transplant unit matron, and Peter Doyle, lead nurse and associate general manager
In the year we celebrate 75 years of our NHS, Helen and Peter Doyle are also marking the 75 years they have worked in this iconic organisation between them.
Helen ‘always wanted to be a nurse’ but Peter says it ‘was the last thing’ he thought he’d do
Helen, matron in Harefield hospital’s transplant unit, says: “I always wanted to be a nurse, I never considered any other type of career.”
But Peter, lead nurse and associate general manager at Harefield has a different story. He recounts: “Nursing was the last thing in the world I thought I’d ever do, but when I was doing my A-levels I volunteered in a hospice run by the catholic church – initially I thought it was awful and I vowed never to go back, but when I was asked to, I was too proud to say no. Bit by bit I got inspired by the people who’d given their lives over to caring for people. I became a healthcare assistant and went on to do my nurse training from there.”
Both Peter and Helen trained at West Middlesex Hospital. Peter and his childhood friend Martin followed an advert in his home town’s paper, the Liverpool Echo, in which the hospital was calling for student nurses. Helen’s journey wasn’t as long: “I wasn’t as adventurous as Pete,” she says. “I looked for something that was far enough away from home to get away but close enough that I return with a bag of dirty washing!”
They met in 1986 at West Middlesex hospital and have been married for 26 years. Peter started working at Harefield in 1996, and Helen in 2003.
Despite describing themselves as “not desperately ambitious”, Peter began his career as an intensive care nurse, and worked his way up to a matron position then a service manager, finally moving away from clinical roles into management. Helen says they both “just wanted jobs we were happy in.” With three small children, she moved to Harefield after finding the juggle of childcare challenging in other hospitals. She says: “I never thought in a million years about applying to the transplant unit because I didn’t have any experience. But I came as a senior staff nurse, then got a sister’s post, and then a matron post seven years ago. I’ve never looked back.”
'One of the beauties about working here are the miracles you see'
Peter and Helen agree that working at Harefield is special. Peter explains: “One of the beauties about working here are the miracles you see. Some of our patients have such a small chance of survival, but here, they do survive.”
Helen says: “There are transplant patients that I looked after 20 years ago when I was a ward nurse and they still come back to see me now when they’re in clinic. Before that transplant they were dying. And we have patients who had a transplant 35 years ago or more, and they’ve gone on to have families, or been able to watch their children or grandchildren grow up.”
'It blew me away how everyone came together during Covid'
Looking back at their careers, Covid, of course, stands out for both Peter and Helen.
Peter says, “Being able to walk around the hospital without a mask on was a good day! The pandemic was rough. But even at the start, when we were all terrified, I kept saying, we’re in the best place. As clinical staff, if we’re going to be anywhere right now, it’s Harefield hospital. We’ll rally together.”
Helen echoes this. “It blew me away how everyone came together during Covid. I remember talk about this new infection, and then all of a sudden it was like a bulldozer. But there was a real team effort here and it reinforced what a great place this is to work.”
Treatments and clinical practices have ‘changed for the better'
Having clocked up 75 years between them, Helen and Peter have seen big changes in clinical practice.
Helen says: “What stands out for me are the ventricular assist devices (VADs). They used to be huge console-like machines that were on wheels. Patients’ hearts would be connected with big thick tubes to a power source and they would have to remain in hospital. Over the years the VADS got smaller and now people can go home and live normal lives.”
For Peter, the primary angioplasty service stands out in his memory: “It was a revolutionary treatment for heart attacks. It seems quite quaint now, the way we used to treat heart attacks with bed rest. Putting tubes down their coronary arteries immediately after a heart attack was unthinkable. But treatment was turned on its head and all of a sudden people recovered more quickly – many even able to go home only after a couple of days after a heart attack.”
They’ve also seen a lot of organisational change.
Peter says, “I began working in intensive care in the 80s – back then it was a new phenomenon but now it’s a vital speciality. I remember it being pretty crude and basic sometimes. One time our charge nurse built a ventilator from scratch with one of our clinical engineers because we just didn’t have enough – regulations were almost non-existent.”
Helen remembers: “It was very hierarchical. As a student you wouldn’t dare call the nurse in charge by a first name, it was always their title. You’d call the consultants ‘sir’. It’s all changed now for the better – you feel like you’re part of one team.”
It’s a family affair
There’s a third Doyle working at Harefield. Helen and Peter’s second son, William, is a patient pathway coordinator for cancer, having previously worked as a porter. Their eldest son also worked as a member of bank staff while studying at university – he’s now a teacher. Their daughter refuses to work in medicine – she studies fulltime in a ballet school.
Both Helen and Peter imagine retiring at Harefield. Helen says: “It’s such a friendly hospital. I can’t see myself anywhere else.”
