Babies and children have different nutritional needs as they're growing, especially if they have heart or lung conditions.
 Children with congenital heart defects, under the care of Royal Brompton, may require modified diets - some temporary and some longer term - because of their medical condition. The dietitian will work with you and medical teams to help your child's help by having a good diet.
Children with congenital heart defects, under the care of Royal Brompton, may require modified diets - some temporary and some longer term - because of their medical condition. The dietitian will work with you and medical teams to help your child's help by having a good diet.
If you are a Royal Brompton patient and require further help or you are worried about your child’s nutrition, please contact us directly for an appointment on:
Respiratory team
Tel: 020 7351 8465
Cardiac team
Tel: 020 7352 8121, ext 2082
If you would like a referral to a dietitian, please contact your consultant or GP.
Weaning
The advice on when to wean your child depends who you talk to or which global/national guideline you've read. In the UK, advice suggests:
Breast milk
Breast milk or formula provides sufficient nutrition for most babies up to six months of age. After this, the milk beings to contain less of the nutrients babies need to keep growing.
Solids
Introduction to solids is recommended at the age of around four to six months (not before 17 weeks) - all babies are different and progress at a different pace, so wait until your baby is ready - look for strong head control and signs that your baby is hungry.
Some evidence suggests that introducing solid food while breastfeeding, at around four to six months, may protect against the development of food allergies. Before four months (17 weeks), evidence suggests the opposite, and that there may be an increased risk of food allergy. There has been no evidence to support the delay of introducing solid foods after six months.
If there's a history of allergies in your family, you may need to introduce foods one at a time, with a gap of three days in between each new food, so it's easier to identify where the reaction may have come from.
Weaning tips:
- introduce solids slowly - start once a day with a little and build the amount gradually
- start with simple foods like baby rice, pureed fruit and vegetables, and introduce a new food every two to three days
- aim to encourage a large variety of different tastes, both savoury and sweet
- carry on breastfeeding, or giving formula milk, throughout - cow's milk can be introduced in cooking from six months
- If you're weaning on a vegetarian diet, make sure plenty of iron-rich vegetarian food is included - these include lentils, beans and smooth nut butters, which can be given from six months if there's no history of allergies in the family
- Be careful about potential choking hazards - always watch your baby when they're eating and pay particular attention to finger food, foods with skin on, and hard foods

Letting your baby lead you
Every parent should make their own decision about what's best for their child.
Baby-led weaning is when your child dictates when weaning should start. By putting pureed and soft, finger food infront of them from the start, they can explore it for themselves. Again, it's important to offer a varied diet including all the food groups and iron-rich sources. Parents often use a combination of both approaches to give the child adequate nutritional intake. It is important to monitor what works best for your child and adapt the approach if needed. For example, if your child finds it difficult to start, you may start with purees and then progress to baby-led weaning.
Website links
- Unicef - weaning leaflet
- The UK Association of Dietitians - weaning fact sheet
New foods
Toddlers go through stages of food refusal, and Neophobia - the fear of new foods - is common at this age. Often, they'll like a food one week and dislike it the next. If your child is reluctant to try new foods, you could try:
- Trying repeatedly - it can take up to 10 exposures to a food before your child accepts it. If they don't like it at first, just try offering it to them another day. In the meantime, you should still carry on offering them a variety of foods so you can keep mealtimes as stress free as possible
- Mixing the new food with a food you already know your child likes. That way, there is something familiar on their plate
- Sticking to a plan. Try to avoid making your child a special meal when they reject a meal or food because this establishes a pattern, in their mind, that they don't need to try new food and they will always get the food they like
- Remaining calm and not reacting if your child refuses to eat the family meal when it's served. You can always put it in the fridge in case they say they are hungry, later
- Not to increase the size of a snack after dinner if they haven't eaten well. You can often get your child interested in what they each by involving them in its creation, such as letting them decide the shape of their sandwich, what plate they want to eat it from, or what shaped pasta they want to each their bolognese with
Help, my child won’t eat or take new foods
When feeding your toddler:
- Offer new foods repeatedly. Children can need to be offered a new food up to 10 times before they will accept and like it.
- Keep mealtimes around maximum 30 minutes.
- Expect and encourage mess. Don’t repeatedly wipe your babies face or hands as this can upset the child and make them stressed at mealtimes.
- It is important to try and keep mealtimes a positive experience. Keep a relaxed environment at the dinner table. Keep the meal a social experience as well as eating and keep conversation varied.
- Praise your child when they eat a new food so that positive attention is associated with eating rather than "trying" to eat.
- Include children in the mealtime process, such as preparing the meal and eating area.
- Children love self-feeding. Try a picnic plate of food they can feed such as ham strips, crackers, soft vegetable sticks with a dip and grated cheese.
- Talk about food in a positive way using words like it "makes you strong" and "gives you energy".
- It can sometimes be helpful to try "star charts". Children respond very well to praise and rewards, such as stickers.
- Recognise the signs for when a child is full and has finished the meal such as turning their head away or pushing food away. Pushing the meal beyond this time increases mealtime stress significantly, often makes feeding more challenging for next time and rarely results in more food taken.
- Aim to offer a varied diet from all the food groups including:
- fruits and vegetables
- breads and cereals
- dairy
- meats, fish and alternatives
- If a child has a really restrictive diet that concerns you please discuss this with your doctor or dietitian.
- Finally, try to be a good role model. If you set a good example following a varied diet when you eat, they are likely to follow.
Cow's milk, formula and other fluids
When can I start using cow's milk?
Cow’s milk can be used from six months of age in the form of dairy products, e.g. yoghurt and cheese, and as part of cooking.
However, cow’s milk should not be used as your baby’s main drink until one year of age. It is preferable to use whole milk for young children, as they require more energy and fat to support healthy growth. You can start using semi-skimmed milk at age two. Skimmed milk should not be introduced before the age of five.
Low-fat dairy products are not suitable for infants and children under two years of age.
Does my child need to change to a stage 2 or toddler formula?
Toddler formulas are not necessary if your child is weaning well and progressing onto solids and finger foods.
Toddler formulas may contain more protein, vitamins and minerals than breast milk or first infant formula but these are not required if your child is receiving these nutrients from food.
My child drinks a lot of juice and no water, should I be concerned?
It is recommended that the beaker is introduced from six months of age.
If your child is having a lot of juice, you may also find this is impacting on their appetite at mealtimes. Water is important in the diet for hydration. However, some children take time to like the taste. We suggest slowly diluting the juice with water or trying squash. This process may take some time. However, it is important to start earlier rather than later as the longer you leave it the more difficult it may become.
Too much juice is associated with dental caries (tooth decay) and diarrhoea. In small quantities, as a part of a balanced diet, there are no concerns.
Food allergies
What if my child has a food allergy?
Being diagnosed with a food allergy can be a stressful occasion. However, with the right diagnosis and management, this stress can be minimised. The current incidence of proven food allergy in children is 6-8 per cent (National Institute for Health and Clinical Excellence, 2011).
It can sometimes be difficult to understand the difference between food allergy and food intolerance. A food allergy is a reaction caused by the immune system to a normally harmless food substance. The body mistakes the food substance as harmful and produces a reaction by the immune system. Reactions vary but can include hives, swelling of the lips, rashes and, rarely, swelling of the tongue and throat, which would restrict airways and require urgent medical attention.
A food Intolerance is when a person has a reaction to a normally harmless food substance that doesn’t involve the immune system and is usually less severe. Intolerance reactions can include abdominal pain and bloating, constipation and headaches.
If you suspect your child has a food allergy, speak to your GP.
When should I introduce solids?
Current research is investigating the ideal timing to introduce solids.
Some of the evidence suggests that introducing solid foods while breastfeeding between the age of four to seven months may have a protective effect against developing food allergies.
Current literature suggests that starting solids before four months (17 weeks) is associated with an increased risk of food allergy.
Research has shown no evidence to support delaying introduction of foods after six months. However, children with a family history of allergies may need to introduce foods one at a time, with a gap of three days in between each new food, so that it is easier to identify any food that causes a reaction.
Website links
Constipation 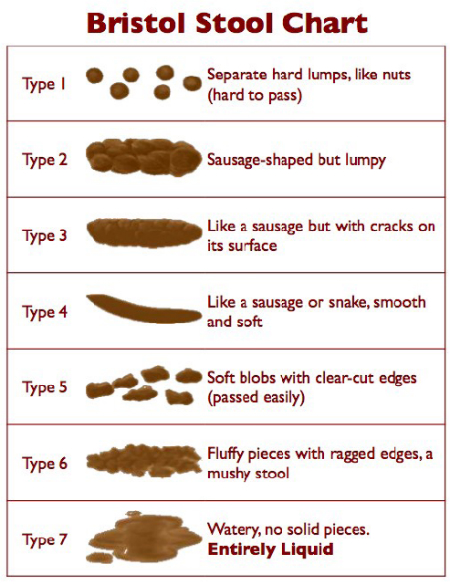
My child is constipated, what can I do?
Constipation is a common complaint raised in child health and not something to be too concerned about.
Everyone has varied stool frequency and the "norm" can vary between three times a day down to once every three days!
If your child’s bowel movements reduce in frequency, they complain of stomach ache, or spend a long time on the toilet, there is most likely a simple explanation.
Read our top tips to maintain regular bowel movements:
- Ensure adequate fluid (6-8 cups of fluid per day)
- Include unprocessed wholegrain as part of a balanced diet
- Aim to have "five-a-day" of fruit and vegetables
- Avoid excessive dried fruit
- Keep moving and get plenty of exercise
- Encourage a bowel routine
Solids, mixed textures and meat
Encouraging your child to eat more solid foods and mixed textures
Mixed texture foods can be a nice stepping stone between puree and finger foods. However, if a child jumps this step and goes straight onto finger foods, this is not a problem.
Often children with a reflux background prefer smooth textures or finger foods.
Encouraging your child to eat meat
Meat is a great source of iron and protein. It may be the texture rather than the taste that the child does not like. Children need repeated exposure to different tastes and textures. If refusal continues, then try softer textures that require less chewing and build up from there. For example, you could try strips of plain omelette or boiled egg, small pieces of vegetarian or meat sausage
Here are some other ideas:
- Slices of ham, corned beef and deli meats cut into strips
- Meat/fish pate or hummus with crackers
- Boiled greens including broccoli or Brussel sprouts
- Dried fruits, including apricots - 1 portion = child's handful
- Beans, such as kidney beans or refried beans spread with cheese or baked beans toastie
- Sardines or mackerel
- Fish fingers or chicken nuggets
- Iron-fortified breakfast cereals
Always try to include vegetables with meat as the vitamin C helps the body absorb the iron.
When is it safe to give my child honey?
Honey should not be given before 12 months due to the risk of infant botulism (bacterial contamination found in honey).
Probiotics and multivitamins
Does my child need probiotics?
The Food and Agriculture Organization of the WHO describes a probiotic as "a live organism that, when ingested in adequate amounts, exerts a health benefit to the host". Probiotic dietary supplements are available in many forms, such as powders, capsules, tablets, chewables, gummies, and liquid. The most commonly used probiotics are short drinks and yogurts, such as Yakult, Actimel, Activia etc. These contain some of the better known organisms called lactobacilli and bifidobacteria.
These are widely available. However, not all of these types of products have been researched or tested enough in humans to demonstrate any particular health benefits. The intestines contain a complex variety of bacteria and the diversity of this is not fully understood. "Good" bacteria will thrive on non-digestible fibre in the diet, also known as prebiotics, and so a healthy gut can be achieved by the majority by eating a varied and balanced diet.
Probiotics may be of benefit following a course of antibiotics to replace all the good bacteria that has been lost in the short term.
Does my child need a multivitamin?
UK national guidelines recommend that all babies aged from six months onwards should be on vitamin supplements to ensure they receive adequate doses of vitamins A, D and C, unless they are drinking 500ml of infant formula a day. 
There are a variety of types readily available, such as "Healthy Start" and "Well Kid" vitamin drops. This can be continued up until your child reaches five years of age.

